What is The Difference Between Dermoscope and Trichoscopy?
Dermoscope and trichoscopy often sound like highly technical tools reserved for specialists, but at their core they are simply smarter ways of looking at the skin and hair. Both rely on a handheld, lighted magnifier to reveal details that our eyes alone can’t see.
In this article, we’ll walk through what dermoscope and trichoscopy actually are, how they differ, and how they’re used in everyday clinical practice—from checking suspicious moles to pinpointing the cause of hair loss and scalp problems.
What is Dermoscope?
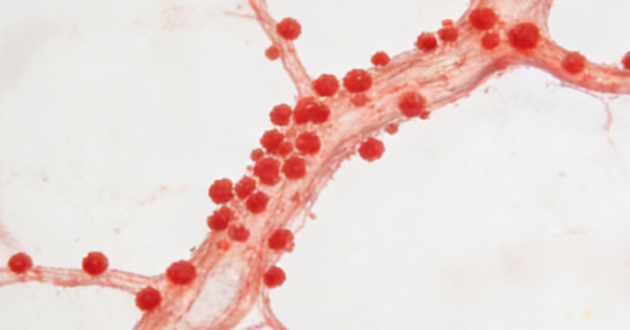
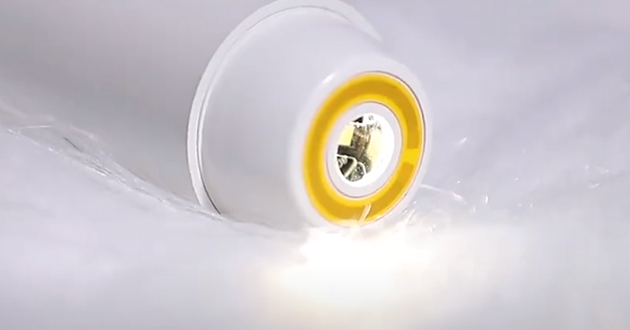
Dermoscopy is a noninvasive way of examining the skin with a handheld device called a dermatoscope. This tool combines magnification with polarized or non-polarized light to reduce surface glare, so structures just beneath the outermost layer of the skin come into view. With roughly 10–20× magnification, clinicians can see fine details in pigment, tiny blood vessels, and scaling that would be invisible to the naked eye.
In everyday practice, dermoscopy tool is most widely used to assess moles and other pigmented lesions, helping doctors judge whether they look harmless or show signs that may suggest melanoma or other skin cancers. It’s also very helpful in evaluating inflammatory skin diseases such as psoriasis, eczema, and cutaneous lupus, where certain dermoscopic patterns can support a particular diagnosis. Many modern dermatoscopes can be connected to cameras or smartphones, making it easy to store images for follow-up, teaching, or telemedicine.

During a dermoscopic examination, the clinician looks not only at how the skin surface appears, but also at the deeper visual patterns within it. They pay attention to the pigment network and how it changes, the shape and distribution of vessels, and the color and pattern of scales, along with other subtle clues that help distinguish one condition from another. In this way, dermoscopy sits between simple visual inspection and a skin biopsy, offering much richer information without needing to break the skin.
What is Trichoscopy?
Trichoscopy is essentially dermoscopy for the hair and scalp. It uses the same type of handheld, lighted magnifier (a dermatoscope), but the focus is on hair shafts, follicular openings, and the surrounding scalp rather than on moles or other skin lesions. In many publications, you’ll also see it referred to as scalp dermoscopy.
In clinical practice, trichoscopy is mainly used to assess hair loss—for example, androgenetic alopecia (pattern hair loss), alopecia areata, telogen effluvium, and different forms of scarring alopecia—as well as scalp conditions such as seborrheic dermatitis, psoriasis, and tinea capitis. By revealing subtle patterns that are invisible to the naked eye, it helps clinicians better understand why a patient is experiencing thinning, shedding, or persistent scalp symptoms like itching and flaking.

The equipment is the same as for dermoscopy: a dermatoscope, which may be handheld or connected to a digital/video system. In many cases, standard magnification is enough; when finer detail is needed, videodermoscopy can provide higher magnification for a closer look at individual hairs and follicles.
During a trichoscopic examination, clinicians usually focus on four main aspects:
Hair shafts – whether hairs are broken, coiled, miniaturized (very fine), or show marked variation in thickness
Follicular openings (ostia) – whether follicles are empty, or show black dots or yellow dots filled with keratin and sebum
Perifollicular skin – signs of redness, scaling, or increased pigmentation around the follicles
Vessels – dotted or linear vessel patterns that may differ between scarring and non-scarring alopecias, or among different scalp diseases
By combining these observations, trichoscope offers a rich amount of diagnostic information with minimal discomfort, often helping to guide decisions and reduce the need for an immediate scalp biopsy.
Dermoscopy Tool vs. Trichoscope
|
Aspect |
Dermoscopy Tool |
Trichoscope |
|
Basic idea |
Non-invasive imaging of the skin using magnification and light |
Same technique applied specifically to hair and scalp |
|
Main target |
General skin surface |
Scalp, hair shafts, hair follicles |
|
Key structures seen |
Pigment patterns, blood vessels, keratin/scale, network structures |
Hair shaft shape/thickness, follicular openings, perifollicular skin, vessel patterns |
|
Typical use cases |
Skin cancer screening, pigmented lesions, inflammatory skin diseases |
Hair loss evaluation, scalp disorders (e.g. dandruff, psoriasis, tinea capitis) |
|
Role in dermatology |
“Generalist” tool for a wide range of skin diseases |
“Specialist” tool focused on hair and scalp problems |
|
Metaphor |
The “parent” technique |
The “child” subspecialty using the same technology |
Dermoscopy tool and trichoscope share the same basic principle but focus on different areas. Both use a lighted magnifier to reveal details that are invisible to the naked eye. The difference is in what they examine: dermoscopy tool is used for the skin as a whole, while trichoscope is dedicated to the scalp, hair shafts, and hair follicles. You can think of dermoscopy as the “parent” technique and trichoscopy as its more focused “offspring,” tailored to explore the causes of hair loss and scalp conditions in greater depth.
How dermoscopy and trichoscopy are used in real life
1. When dermoscopy comes into play
New or changing mole
A patient notices a new pigmented spot, or a mole they’ve had for years starts to change in size, color, or shape. In this situation, dermoscopy allows the clinician to closely examine pigment structures and vessel patterns within the lesion. These details help determine whether it looks like a benign nevus or shows features that raise concern for melanoma and should be biopsied.

Red, scaly plaques on the body
Another typical scenario is someone with widespread red, scaly patches on the trunk or limbs. Using dermoscopic, the doctor can evaluate vascular patterns, background color, and how the scale is arranged to help distinguish psoriasis from eczema or other types of dermatitis.
In more extensive disease, such as erythroderma (where most of the skin is red and peeling), dermoscopic patterns may still suggest certain causes—like psoriasis, pityriasis rubra pilaris, dermatomyositis, or crusted scabies—while others remain difficult to separate and still need confirmation through clinical evaluation, biopsy, and laboratory tests.
If you want to read more about this,you can click it:
https://pubmed.ncbi.nlm.nih.gov/33073390/
2. When trichoscopy takes the lead
Androgenetic alopecia (pattern hair loss)
A patient reports gradually thinning hair over the frontal or vertex scalp. Trichoscopy may reveal hairs of unequal thickness, numerous fine miniaturized hairs, yellow dots, and empty follicles. Together, these findings support a diagnosis of pattern hair loss and provide a baseline for monitoring how well treatment is working.
Alopecia areata
In alopecia areata, a sharply defined bald patch often appears quite suddenly. Under trichoscopy, the clinician may see black dots, yellow dots, “exclamation mark” hairs, and short regrowing hairs. This pattern is highly suggestive of alopecia areata and helps differentiate it from hair loss caused by breakage or traction.

Scarring alopecia
If hair loss areas are irregular and accompanied by burning, tightness, or discomfort, scarring alopecia becomes a concern. Trichoscopy can show loss of follicular openings, white structureless areas or dots, and specific vascular patterns. These clues point toward permanent follicular damage and usually prompt early biopsy and intervention.
Heavy dandruff with an unclear cause
A patient might present with persistent flakes and redness on the scalp, and it’s not immediately clear whether this represents seborrheic dermatitis or scalp psoriasis. Trichoscopy lets the clinician compare scale thickness and color, vessel patterns, and changes around the follicles. These subtle differences can shift the diagnosis toward one condition or the other. In patients with very widespread redness and scaling, similar trichoscopic features—such as particular vessel types and pale or pink structureless areas—can also help narrow down the underlying disease.

Read more:
https://www.djmimoreme.com/resources/blog/how-accurate-are-dermatoscopes.html
https://www.djmimoreme.com/resources/blog/can-a-dermoscopy-detect-cancer.html
Conclusion
Understanding how these tools are used doesn’t replace a medical consultation, but it can make clinic visits less mysterious. The next time your dermatologist reaches for a dermatoscope, you’ll know that this small device is providing a large amount of extra information—often helping to refine the diagnosis, guide treatment, and sometimes avoid unnecessary biopsies.
Table of Contents
Related information
How can we help you?
Have specific questions or requests? Fill out our inquiry form, and our dedicated team will get back to you promptly. Your inquiries are important to us, and we are committed to providing comprehensive and personalized responses tailored to your needs.











 Reach out to us today!Whether you are preparing to start your own
business in the beauty industry, are ready to upgrade your
equipment, or are just interested in our products,Contact us
today, and let’s explore how we can partner to achieve your goals
and drive your success to new heights!
Reach out to us today!Whether you are preparing to start your own
business in the beauty industry, are ready to upgrade your
equipment, or are just interested in our products,Contact us
today, and let’s explore how we can partner to achieve your goals
and drive your success to new heights!
