How Accurate are Dermatoscopes ?
In this article, we’ll look at how dermatoscopes vary in accuracy, what influences that accuracy (from lesion type to user expertise and device quality), and the key limitations and considerations that both clinicians and patients should keep in mind. The goal isn’t to oversell dermoscopy, but to give a realistic picture of what it can do—and what it can’t.
How Dermatoscopes Vary in Accuracy
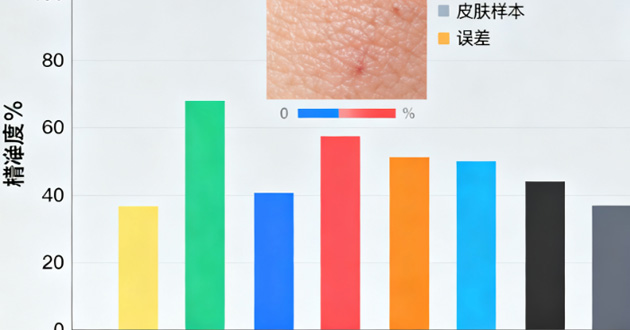
Dermatoscopic accuracy is dynamic rather than absolute—it changes based on lesion type, practitioner expertise, device quality, and the broader clinical context. Understanding these variables helps set realistic expectations about what dermatoscopy can and cannot achieve.

Accuracy of Dermascope in Different Skin Lesion Types
Dermatoscopes are powerful tools, but their diagnostic performance isn’t equal across all skin lesions. The nature of the lesion largely determines how much accuracy can be achieved.
Melanoma Detection
|
Dimension |
Details |
Clinical Significance |
|
Sensitivity Improvement |
Dermatoscopy improves early melanoma detection, with around 20–30% higher sensitivity than naked-eye exam. |
Helps find melanoma earlier and more reliably. |
|
Visualization of Subtle Patterns |
Shows atypical pigment networks, irregular streaks, regression areas, blue-white veils, etc. |
Makes crucial early warning signs visible. |
|
Early Detection Confidence |
Increases confidence before obvious surface changes appear. |
Enables treatment at an earlier, more curable stage. |
Benign vs. Malignant Differentiation
|
Dimension |
Details |
Clinical Significance |
|
Differentiation Capability |
Helps distinguish benign lesions (e.g., nevi, seborrheic keratoses) from malignant ones (e.g., melanoma, BCC). |
Supports more accurate diagnosis and fewer errors. |
|
Key Structures Visualized |
Reveals pigment networks, dots/globules, pseudopods, vessels, and keratin. |
These patterns guide risk assessment of lesions. |
|
Diagnostic Value |
Allows more precise lesion classification and fewer unnecessary biopsies. |
Improves accuracy while limiting overtreatment. |
Non-Pigmented Lesions
|
Dimension |
Details |
Clinical Significance |
|
Diagnostic Challenge |
Amelanotic lesions lack pigment patterns and are harder to read. |
Increases complexity of diagnosis. |
|
Dependence on Vascular Patterns |
Strongly relies on vascular morphology and expert interpretation. |
Requires experienced clinicians to avoid errors. |
|
Accuracy Levels |
Accuracy is lower than for pigmented lesions. |
Dermatoscopy is helpful but not perfect here. |
|
Advantage Over Naked-Eye Exam |
Still more accurate than visual inspection alone. |
Even challenging lesions benefit from dermoscopy. |

Impact of User Expertise
With dermatoscopes, the person behind the device is just as important as the device itself. A dermatologist who uses dermoscopy every day learns to notice the small things—slight changes in pigment, unusual networks, or that subtle “something’s off” feeling—that a less experienced clinician might overlook. After examining thousands of lesions, they develop an almost automatic sense of pattern recognition: which spots are likely harmless, which are worth keeping an eye on, and which really shouldn’t wait for a biopsy.

General practitioners and other non-specialists can still benefit from using a dermoscopic, but their accuracy is often less consistent. As one Reddit user bluntly put it, “Not every derm knows how to actually use a scope properly — they just glance and move on.” That sentiment reflects many patients’ experiences: the tool itself is helpful, but what really matters is how often the clinician uses it, how much time they spend examining you, and whether they’ve had solid dermoscopy training.
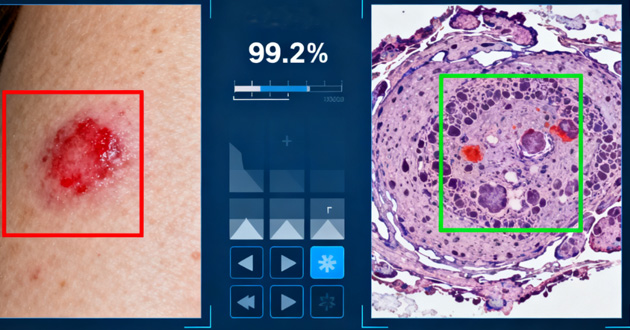
AI-assisted dermatoscopy is starting to help fill some of these gaps. Digital systems and smartphone-based tools can compare your lesion with large image databases and flag areas that might deserve a closer look, which can be especially useful when the clinician is less experienced. But AI has clear limits: it depends on good images, proper technique, and diverse training data, and it still doesn’t know your personal context—your history, symptoms, or risk factors. As another Reddit commenter summed it up, “The tech is cool, but it can’t replace a trained pair of eyes.”
From a user’s perspective, the ideal situation is clear: a well-trained clinician who uses a good dermatoscope regularly, may use AI as a helpful extra pair of “digital eyes,” and ultimately makes decisions based on your whole clinical picture—not on the device alone.
If you want to learn more about the content of reddit posts, click this:
Dermoscopy Tools Limitations and Considerations
Dermatoscopes are incredibly helpful in everyday practice, but they’re not magic wands. Even with the best dermatoscope, there are real limits to what dermoscopy can do. Understanding these boundaries helps avoid misreading findings, overconfidence, and giving patients false reassurance.
1. Dependence on Operator Skill
Dermoscopy is first and foremost a visual interpretation skill, not just a function of owning a good dermatoscope. Everything depends on how well the clinician can recognise and interpret dermoscopic patterns. Without solid training and regular hands-on use, harmless lesions can be labeled “suspicious”, while genuinely dangerous ones—especially atypical or amelanotic melanomas—may slip through. In practice, the “accuracy” of a dermatoscope usually reflects the experience, education, and routine use of the person behind it.
2. Not a Replacement for Biopsy
A dermatoscope is excellent for answering, “Does this look worrying enough to investigate further?”—but it cannot definitively answer, “What exactly is this lesion?” When skin cancer is a concern, biopsy and histopathology remain the final authority. Even if a lesion looks relatively reassuring under dermoscopy, factors like patient history, evolution over time, or gut feeling may still make sampling or removal the safer option. Dermatoscopes guide decisions; they don’t replace tissue diagnosis.
3. Variability in Image Quality
What dermoscopy reveals is only as good as the image the clinician creates with the dermatoscope. Poor lighting, shallow contact with the skin, the wrong angle, or slight motion blur can all obscure key structures. This becomes even more important with digital dermatoscopes, where images are saved, compared, or shared later. Consistent technique, good contact, and careful image capture are essential to maintain confidence in dermoscopic findings.
4. Over-reliance on AI Tools
AI-powered dermatoscope apps and software are evolving quickly, and they can be very useful as an extra layer of analysis. But they’re not foolproof. Performance can drop with rare lesion types, certain skin tones, or low-quality photos. And unlike a real consultation, AI doesn’t “see” the whole patient—it can’t factor in personal history, medications, or subtle symptoms. Used well, AI in dermoscopy works best as a supportive second opinion, not as a standalone diagnostic decision-maker.
5. Certain Lesion Types Remain Challenging
Even in expert hands with a high-quality dermatoscope, some lesions are genuinely tricky. Amelanotic and nodular melanomas may lack the classic pigment patterns dermoscopy relies on, while benign conditions like seborrheic keratoses, dermatofibromas, or vascular lesions can look alarmingly similar to malignancies. In these gray zones, dermoscopy is just one part of the puzzle—alongside clinical judgement, follow-up, and, when uncertainty remains, biopsy.
https://www.djmimoreme.com/resources/blog/top-5-best-dermatoscope-in-2025.html
https://www.djmimoreme.com/resources/blog/top-5-skin-analysis-machines-in-the-usa-2025-guide.html
Conclusion
Dermatoscopes clearly raise the standard of skin and scalp examination: they help catch melanoma earlier, distinguish many benign from malignant lesions more confidently, and support better long-term monitoring. But their accuracy is not fixed. It depends on what is being examined, who is using the dermatoscope, what device is chosen, and how the findings are interpreted in context.
Table of Contents
Related information
How can we help you?
Have specific questions or requests? Fill out our inquiry form, and our dedicated team will get back to you promptly. Your inquiries are important to us, and we are committed to providing comprehensive and personalized responses tailored to your needs.











 Reach out to us today!Whether you are preparing to start your own
business in the beauty industry, are ready to upgrade your
equipment, or are just interested in our products,Contact us
today, and let’s explore how we can partner to achieve your goals
and drive your success to new heights!
Reach out to us today!Whether you are preparing to start your own
business in the beauty industry, are ready to upgrade your
equipment, or are just interested in our products,Contact us
today, and let’s explore how we can partner to achieve your goals
and drive your success to new heights!
